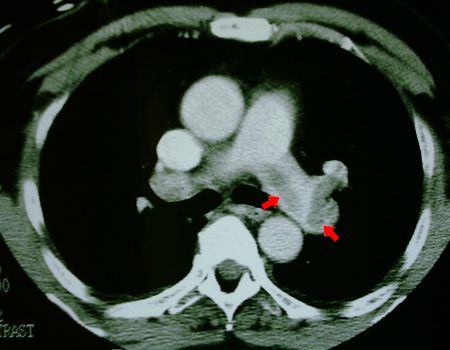
Fig 1. Spiral CT of patient showing large thrombus (arrowed) within the left pulmonary artery
When confronted with a patient with a large, documented pulmonary embolus who has indications and contraindications for thrombolysis, direct intra-embolic thrombolytic infusion may be life-saving.
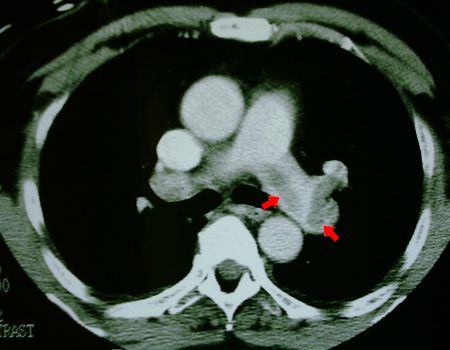
Fig 1. Spiral CT of patient showing large thrombus (arrowed)
within the left pulmonary artery
Arterial blood gas analysis on an FiO 2 of 90% breathing spontaneously with a respiratory rate of 35/min, showed a pH of 7.47, PaCO 2 of 31 mmHg (4.0 KPa), PaO 2 58 mmHg (7.6 KPa). Note that this is at an altitude of 1600m. Blood pressure was 100/60, heart rate 90/min. Urine output averaged 80 ml/hr. The patient was distressed and tiring.
Because of the recent craniotomy, conventional thrombolysis was contra-indicated. We felt that standard anticoagulation was insufficient in the face of the patient's hypoxaemia and general clinical status. A pulmonary artery catheter (PAC) was advanced into the thrombus in the right pulmonary artery, with screening. Ten milligrams of recombinant human tissue plasminogen activator (rTPA) was infused over ten minutes via the PAC. No improvement was noted, so a further 10mg of rTPA was given via the same route, after repositioning the catheter within the clot. A dramatic improvement in arterial saturation (from 85% to 95%) was seen on pulse oximetry. No further thrombolysis was administered.
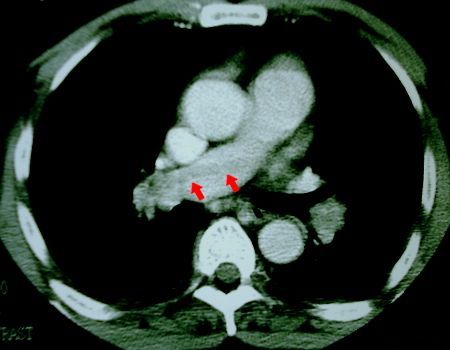
Fig 2. CT showing long thrombus extending
into right pulmonary artery.
Following the procedure, on an FiO 2 of 70%, the pH was 7.47, PaCO 2 31 mmHg, and PaO 2 was 85 mmHg (11.2 KPa). The patient looked dramatically better, and his respiratory rate had decreased to 20 /min. Urine output increased to 220 ml/hr, but this may in part have been related to the administration of radiological contrast medium. His aPTT was maintained at twice normal using a carefully monitored infusion of unfractionated heparin, with no bleeding complications. The patient was discharged well eight days later, on warfarin.
Although intellectually appealing, intra-pulmonary arterial infusion of thrombolytics is generally considered to be a waste of time. There appears to be only one randomised controlled trial comparing intrapulmonary arterial infusion of throbolytics with peripheral infusion - that of Verstraete et al (Circulation 1988 Feb 77.2 353-0). In this study, there were no significant differences between patients given intrapulmonary arterial versus intravenous thrombolytics, in 34 patients. Inclusion criteria were over 48% vascular occlusion; 50mg was given over 2hr and then 50mg over 5hr in select patients. from these data it has been concluded that there is no advantage to giving thrombolytics by pulmonary artery infusion.
In experimental models of pulmonary thromboembolism, direct intra-embolic infusion of thrombolytics has enhanced thrombolysis (Tapson V et al, ARRD 1991 143 A668). Tapson et al (Chest 1994 106 1558-2) in another study suggest that the mechanical effects of the catheter may also improve thrombolysis. Such studies have spearheaded the drive to use this approach clinically, especially where there is a relative contra-indication to the use of high-dose thrombolytics.
Several small studies suggest that infusion of thrombolytics into the pulmonary arterial circulation is effective and fairly safe. The most promising agents appear to be urokinase or rTPA. Dramatic improvement has been noted following doses of 10 to 20mg of rTPA, or 250 000 to 500 000 units of urokinase (about ten to twenty percent of conventional doses). The following studies used infusion of thrombolytics directly into the thrombus :
The role of intra-embolic infusion of thrombolytics is far from clear. Routine PAC insertion and thrombolytic infusion following diagnosis of pulmonary embolism seems inappropriate. We recommend that the procedure be used in massive pulmonary embolus with contra-indications for systemic thrombolytic therapy. By "massive" we mean that there is profound respiratory or cardiovascular compromise. The therapy must still be regarded as experimental, but may be life-saving.
B. Traub
M.J. Hopley
J. van Schalkwyk
| Date of First Publication: 2000/1/10 | Date of Last Update: 2006/10/24 | Web page author: Click here |